The Preferred Resource for
USMLE® Step 3 Preparation &
CCS Cases
- 2,100+ questions and 90+ CCS cases
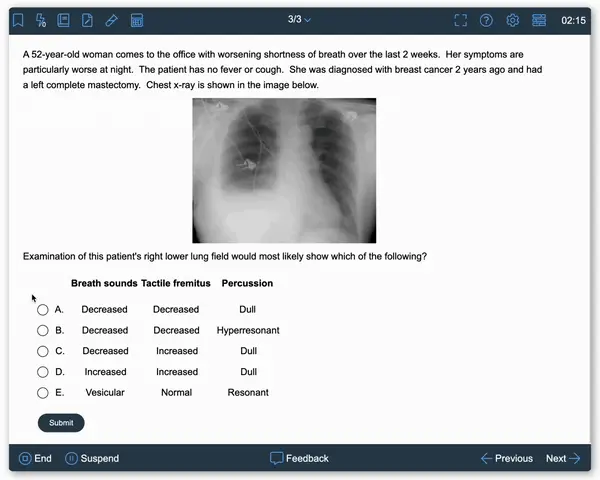
- Based on real-life clinical scenarios
- Paired with in-depth, visual answer explanations
- Tested in an exam-like software interface
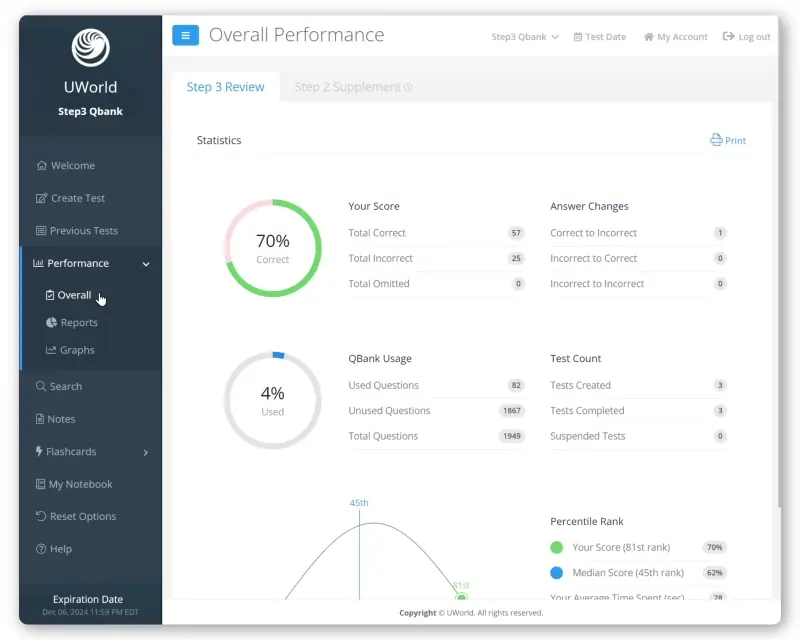
- Organized to track your performance by subject and system
Complete the USMLE with Our Proven Step 3 Prep
Our Step 3 QBank delivers realistic practice questions and Computer-based Case Simulations (CCS cases) to reflect what residents will experience on their final USMLE exam. By choosing UWorld, you’ll receive high-yield content and time-saving study tools to improve your clinical skills ahead of licensure.
Finding the time to study for Step 3 during residency is challenging, which is why choosing a comprehensive, yet concise medical learning solution is a must. We give you the flexibility to study at home or on the go, and regularly update our material to reflect the latest content outline.
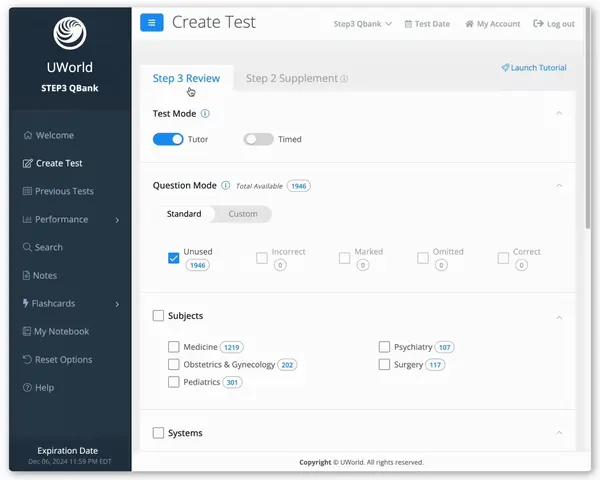
Study Your Way with Our Step 3 Question Bank
To make your prep more efficient, we built our Step 3 QBank to be as customizable and adaptable as possible. Our goal is to empower your study preferences to get you across the finish line and set you up for a successful career in medicine.
Create custom tests and quizzes with dedicated Step 3 practice questions in “Step 3 Review.” Any content outline updates will be found here, such as the exam’s recent focus on basic sciences questions. We also offer “Step 2 Supplemental” questions to refresh your knowledge of key concepts tested on both exams. All of our Step 3 questions feature detailed, visually rich explanations written by practicing physicians.
Increase your retention by taking an active role in your learning. Simply highlight high-yield text and graphics from our answer explanations to create custom flashcards and digital notes. You can then rewrite and summarize our material in your own words for later review.
UWorld Step 3 Success Stories






Beyond Our Step 3 QBank
Once you become familiar with our Step 3 question bank and active-learning tools, we encourage you to explore our CCS cases, self-assessments, biostatistics review, and mobile app. Each serves a specific purpose in furthering your clinical development and making your Step 3 preparation more efficient.
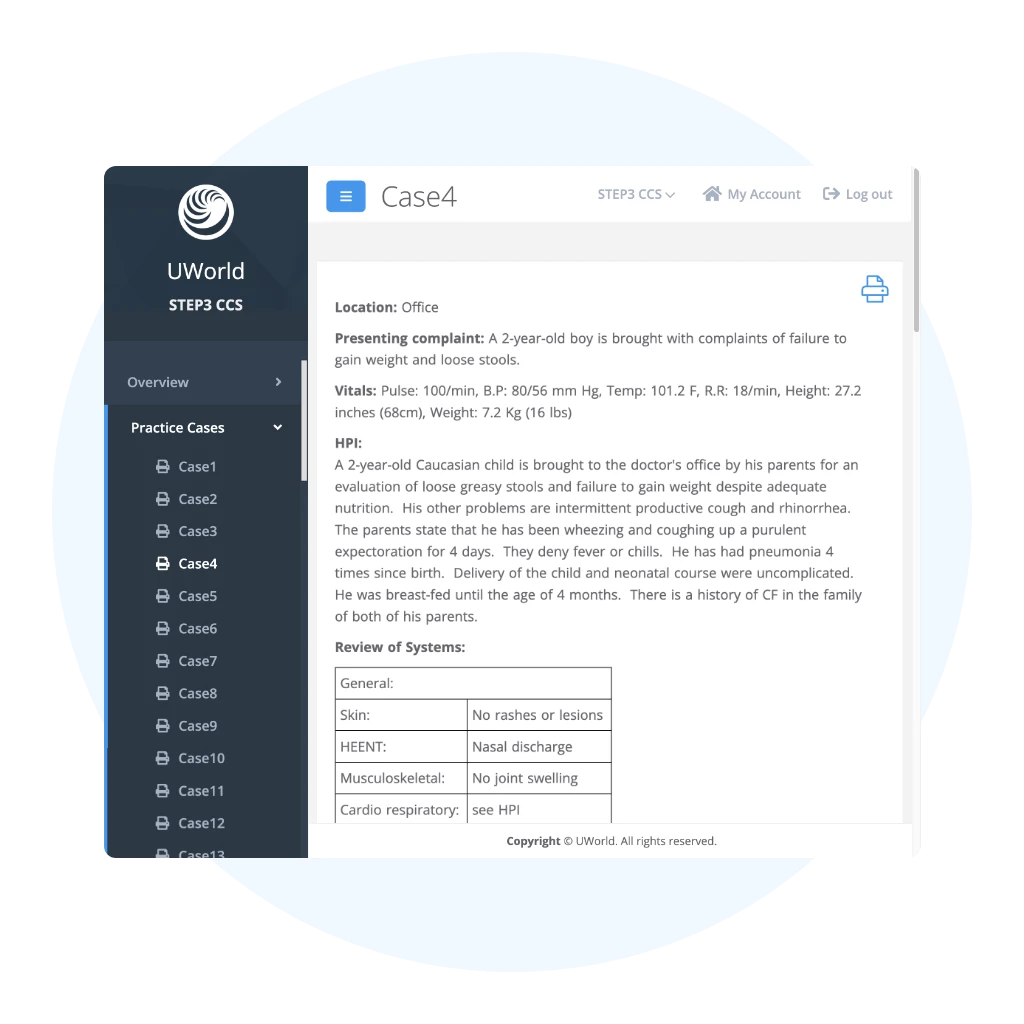
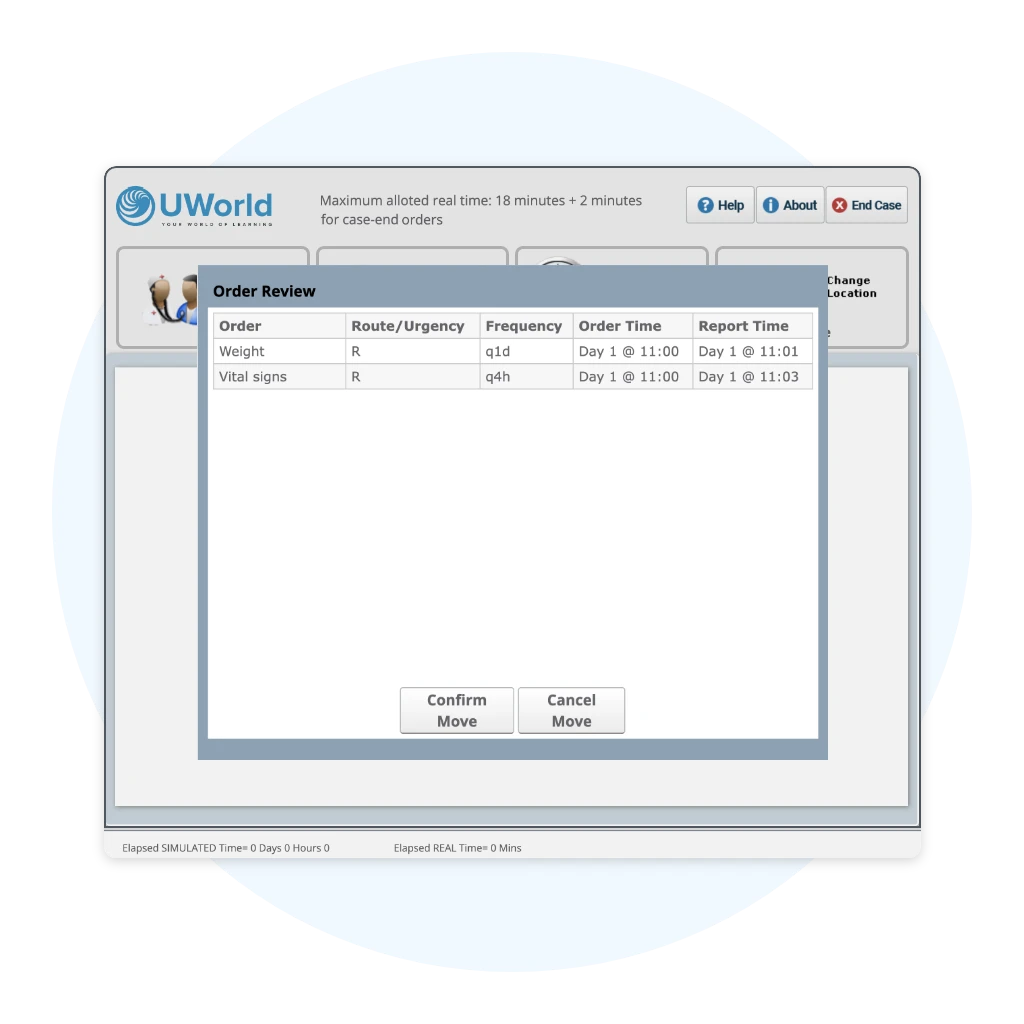
Computer-Based Case Simulations
UWorld Step 3 CCS cases evaluate your ability to diagnose, treat, and monitor simulated patients in an interactive setting. Familiarity with this interface is crucial to improving your score on this section of the exam. Our first-of-its-kind Step 3 CCS software features:
- 40+ classic Step 3 CCS cases that cover essential topics in multiple specialties
- 50+ interactive cases that closely mimic highly tested Step 3 topics
- An interface that uses free-text order entry similar to what’s found on the actual exam
- Comprehensive explanations that include tips on the recommended clinical approach, scoring features, and clock management
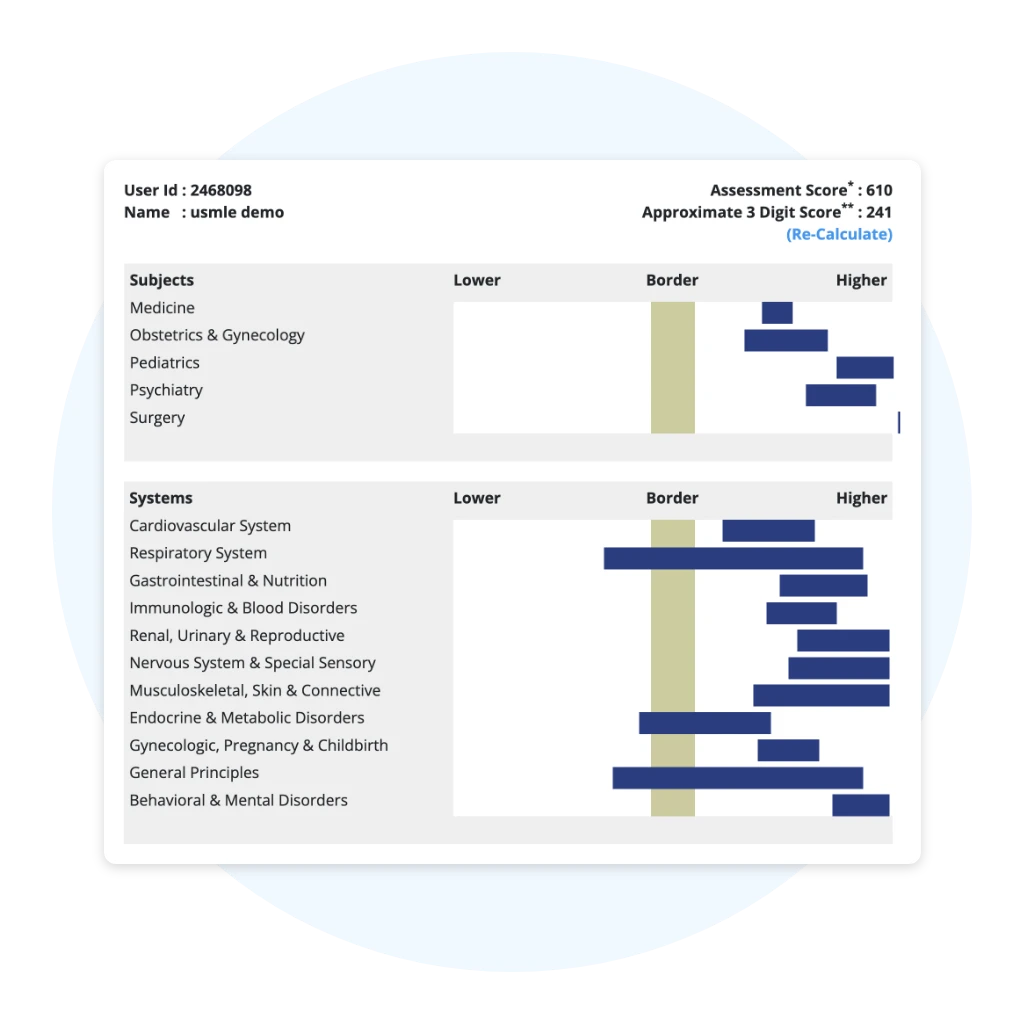
Step 3 Practice Tests
UWorld Step 3 self-assessments closely replicate the experience of the official Step 3 exam to help you prepare for test day. Each self-assessment consists of four 60-minute blocks containing 40 unique multiple-choice questions. These questions cannot be found in our QBank. Once completed, you can review:
- Detailed explanations for each question, including vivid illustrations and charts
- Performance analytics and your relative ranking compared to other residents
- An approximate 3-digit USMLE score based on historical UWorld data
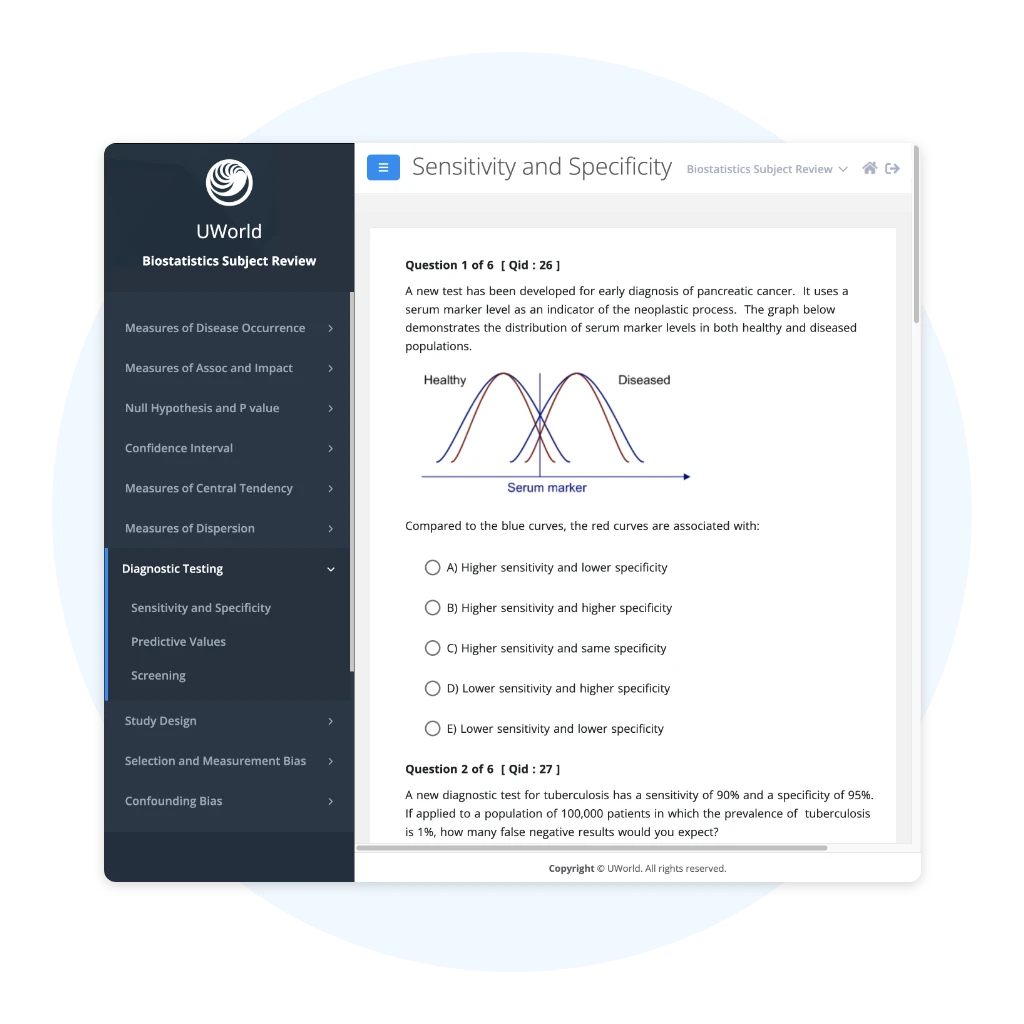
Biostatistics Review
Biostatistics and epidemiology are essential to performing well on the USMLE and becoming a successful physician. Our review will help you:
- Learn important concepts and strengthen your fundamental knowledge
- Apply content in exam scenarios through vignettes
- Learn and apply step-by-step calculations
- Integrate material from multiple questions to increase your comprehension
Study from Anywhere
We’ve been in your shoes and understand how valuable your time is as a resident. That’s why we developed our Step 3 QBank and CCS cases to be fully configurable on your smart devices. Simply download the UWorld Medical app for a seamless study experience. All of your data will be automatically saved and synced.
USMLE Step 3 QBank Pricing
Questions about subscriptions/renewals? Click here.
QBank & CCS
(90 Days each)
429
- Full QBank Access
- 2 Self-Assessments*
QBank, CCS, & Biostats
(180 Days each)
479
- Full QBank Access
- 2 Self-Assessments*
- One-time Reset Option
QBank, CCS, & Biostats
(360 Days each)
579
- Full QBank Access
- 2 Self-Assessments*
- One-time Reset Option
*Each self-assessment has a duration of two weeks from its date of activation.
Biostatistics Review
90-Day Access
25
- Fast and effective way
to learn biostatistics and epidemiology concepts
QBank
7-Day Renewal
59
- 7-Day Access Extension
QBank
15-Day Renewal
89
- 15-Day Access Extension
QBank
30-Day Renewal
149
- 30-Day Access Extension
QBank
60-Day Renewal
219
- 60-Day Access Extension
QBank
90-Day Renewal
259
- 90-Day Access Extension
QBank
180-Day Renewal
319
- 180-Day Access Extension
QBank
360-Day Renewal
399
- 360-Day Access Extension
CCS
7-Day Renewal
35
- 7-Day Access Extension
CCS
15-Day Renewal
55
- 15-Day Access Extension
CCS
30-Day Renewal
75
- 30-Day Access Extension
CCS
60-Day Renewal
95
- 60-Day Access Extension
CCS
90-Day Renewal
115
- 90-Day Access Extension
CCS
180-Day Renewal
135
- 180-Day Access Extension
CCS
360-Day Renewal
155
- 360-Day Access Extension
Form 1 Assessment
2-Week Renewal
30
- 2-Week Access Extension
Form 2 Assessment
2-Week Renewal
30
- 2-Week Access Extension
Biostatistics Review
90-Day Renewal
20
- 90-Day Access Extension
Step 3 Institutional Pricing
We partner with academic institutions to provide bulk pricing on the industry’s highest-quality medical exam prep solutions. We’ll work with you to create a package that enhances your medical program.